Employers recognize that for too long, health care costs have risen without commensurate improvement in health outcomes. With their investments in health care totaling $1 trillion annually, employers can and should expect better value for health care – particularly when it comes to quality of care.
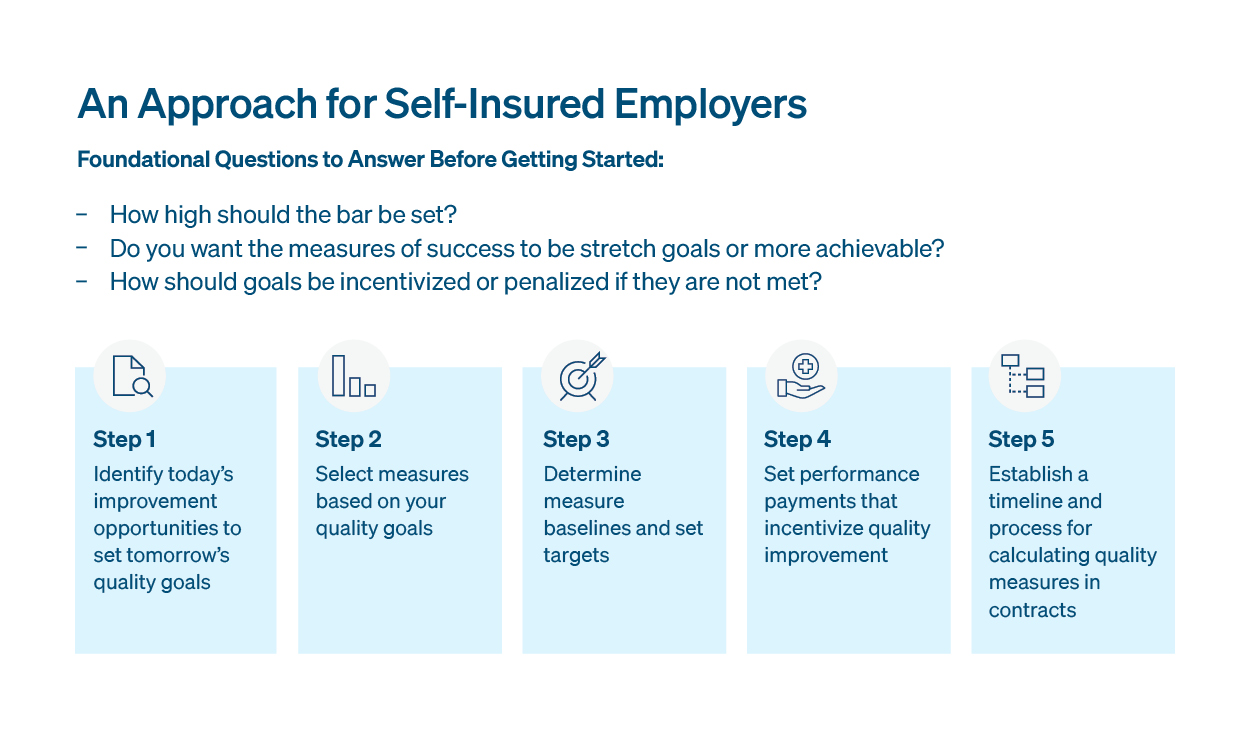
Tying incentive payments to clinical quality measures or putting fees-at-risk for performance targets are ways to hold health plans, providers, and point solution vendors accountable for achieving quality standards.
“When payments are tied to performance, employers can feel more confident that covered health care providers will focus on improving clinical outcomes and employee health,”
Fatema Salam, Vice President and Quality Lead, Morgan Health
The reality, though, is that integrating quality measures into contracts in the form of outcomes-based performance guarantees is not common practice the benefits ecosystem – despite a growing desire from employers to prioritize quality. Morgan Health’s learnings from a recently conducted series of interviews with self-insured employers underscored that employers want to learn from other employers through open access to best practices that provide details around what worked or did not work when integrating accountability for health outcomes. To support this shift, more collaboration and transparency is needed across the employer sector.
"With 285,000 lives covered through our benefits plan, we're dedicated to sharing our learnings to help our industry peers drive greater value from their benefit offerings,"
Dotan Ziv, Head of U.S. Benefits Design and Strategy, JPMorganChase
In that spirit of transparency and collaboration, Morgan Health, with its partners in JPMorganChase Benefits, developed and is implementing a data-driven and measurable approach to quality improvement. We identify, prioritize and integrate measures into contracts that improve quality across four domains: health improvement, access to care, effective chronic condition management and reducing disparities. It’s our intent that our experience offers a roadmap for how employers can drive quality improvement and better health outcomes for their employees.
Read the full approach – along with actionable guidance for employers to consider here. As we continue to share insights, we invite other employers to participate and share best practices across the sector – and we look forward to being open and transparent about our progress.
Quality Measures and Improvement